Vascular Inflammation vs. Infiltration: Origin, Signs, and Remedies
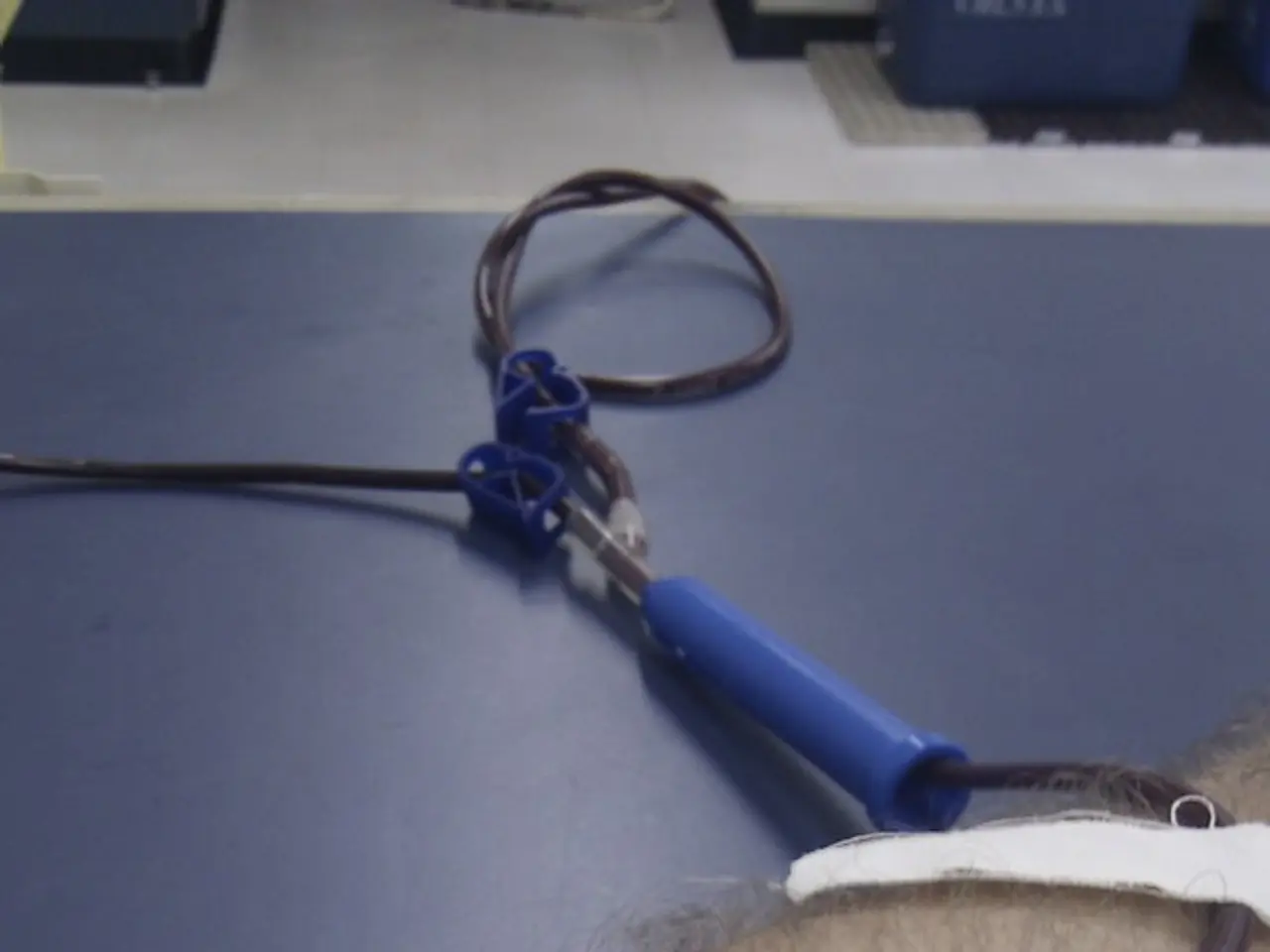
Intravenous (IV) therapy is a common medical procedure, but it can come with complications. Two such complications are phlebitis and infiltration, which affect the vein and surrounding tissue.
Phlebitis and infiltration differ in their symptoms, treatment, prevention, and outlook.
Phlebitis, an inflammation of the vein, is characterized by redness, warmth, swelling, and pain along the vein. Infiltration, on the other hand, occurs when IV fluid leaks into the surrounding tissue, causing swelling, pallor, coolness, and discomfort at the site, but usually without inflammation of the vein itself.
Treatment for phlebitis includes removing the IV catheter, applying warm compresses, and using topical agents like ichthammol glycerin or heparinoids to reduce inflammation and pain. Ichthammol glycerin was found to be more effective in reducing symptoms. Infiltration treatment requires immediate cessation of the IV infusion, limb elevation, cold compresses for mild cases, and interventions to prevent tissue damage from irritant fluids in severe cases.
Prevention for both conditions involves proper IV technique, secure catheter fixation, regular site assessment during therapy, and timely catheter removal or change. Phlebitis prevention focuses on minimizing vein irritation and infection, while infiltration prevention focuses on ensuring catheter placement and function within the vein.
The outlook for phlebitis is usually self-limiting with appropriate treatment, but it can lead to thrombophlebitis if untreated. Infiltration generally resolves without long-term effects unless extravasation of vesicant drugs causes tissue necrosis.
Despite their differences, both phlebitis and infiltration share some similarities. They both occur as IV therapy complications involving the vein and surrounding tissue. Both require cessation of IV infusion upon detection and immediate intervention. Pain and swelling at the IV site are common signs in both conditions. Prevention through skilled IV insertion and ongoing monitoring is critical for both.
It's important for the person receiving treatment to understand both conditions. Infiltration may cause symptoms such as pain, swelling, blistering, blanching of the skin, tingling, numbness, reduction in temperature, sensitivity at the IV insertion site, and signs of infection. In severe cases, infiltration may cause complications such as poor circulation and tissue death. The person must understand infiltration and remove the catheter at the first signs of infiltration to prevent inflammation and complications.
Frequently checking the area of the IV insertion and surrounding areas is important to prevent infiltration. Risk factors for infiltration include placement of a catheter into an area with only a small amount of soft tissue, large needle size, and frequent insertion of a cannula.
Risk factors for phlebitis include long IV therapy, presence of bacteria or viruses, site of catheter insertion, duration of IV therapy, antibiotic use, assigned sex at birth, number of puncture sites, and emergency intervention.
Prevention methods for phlebitis may include monitoring and evaluating IV treatment, keeping records, removing the catheter if signs of phlebitis appear, changing catheters and dressings as necessary, avoiding certain insertion sites, using antiseptic solutions, maintaining proper handwashing and using gloves, good communication between healthcare professionals and the person receiving treatment, and consulting the person about the location of the catheter insertion, explaining signs of phlebitis, and checking for discomfort or symptoms.
In summary, phlebitis is an inflammatory reaction within the vein, while infiltration involves leakage of IV fluid into tissues. Treatment and outlook differ accordingly, but prevention and early detection share many principles. The choice of topical treatment in phlebitis can affect recovery speed, with ichthammol glycerin showing effectiveness in symptom reduction. Early recognition and prompt action can help prevent both complications.
- Phlebitis, an inflammation of the vein, often presents with symptoms such as redness, warmth, swelling, and pain along the vein.
- Infiltration, on the other hand, occurs when IV fluid leaks into the surrounding tissue, causing symptoms including swelling, pallor, coolness, discomfort, but usually without inflammation of the vein itself.
- Treatment for phlebitis includes removing the IV catheter, applying warm compresses, and using topical agents like ichthammol glycerin or heparinoids.
- Infiltration treatment requires immediate cessation of the IV infusion, limb elevation, cold compresses for mild cases, and interventions to prevent tissue damage from irritant fluids in severe cases.
- Prevention for both conditions involves proper IV technique, secure catheter fixation, regular site assessment during therapy, and timely catheter removal or change.
- The outlook for phlebitis is usually self-limiting with appropriate treatment, but it can lead to thrombophlebitis if untreated.
- Risk factors for phlebitis include long IV therapy, presence of bacteria or viruses, site of catheter insertion, duration of IV therapy, antibiotic use, assigned sex at birth, number of puncture sites, and emergency intervention.