Strategies when Enzyme Replacement Therapy Failure Occurs
Adjusting Pancreatic Enzyme Replacement Therapy (PERT) Dosage for Exocrine Pancreatic Insufficiency (EPI)
For individuals living with Exocrine Pancreatic Insufficiency (EPI), managing symptoms requires careful attention to their Pancreatic Enzyme Replacement Therapy (PERT) dosage.
PERT dosage may need to be adjusted based on meal size, fat content, and the patient's response to treatment. A standard initial dose should be used as a starting point, but further adjustments may be necessary if symptoms such as steatorrhea, bloating, and abdominal discomfort persist.
The dosage should be titrated according to symptoms. If patients still experience symptoms, the enzyme dose can be increased gradually while monitoring improvement. Many patients may initially require doses higher than standard recommendations to normalize symptoms and nutrient absorption.
Dietary factors also play a crucial role in determining the appropriate PERT dosage. Larger or higher-fat meals may require greater enzyme doses, while eating smaller, more frequent meals or adjusting fat intake can affect enzyme needs and symptom control.
Tools like the EPI/PEI Symptom Score (EPI/PEI-SS) can help quantify symptom severity and guide dose adjustments. The goal is to help patients achieve scores within the non-EPI symptom range.
Persistent symptoms and nutrient deficiencies despite PERT may indicate the need for higher doses or closer clinical monitoring. In such cases, it's essential to assess nutritional status and inflammation markers.
It's crucial to consult healthcare providers or pharmacists experienced with PERT for personalized dosing, especially in complex cases or those with coexisting conditions like sepsis or chronic pancreatitis.
In summary, adjusting PERT dosage is a dynamic and patient-specific process driven by ongoing assessment of symptoms, meal composition, and nutritional markers to ensure adequate enzyme replacement and symptom control in EPI patients.
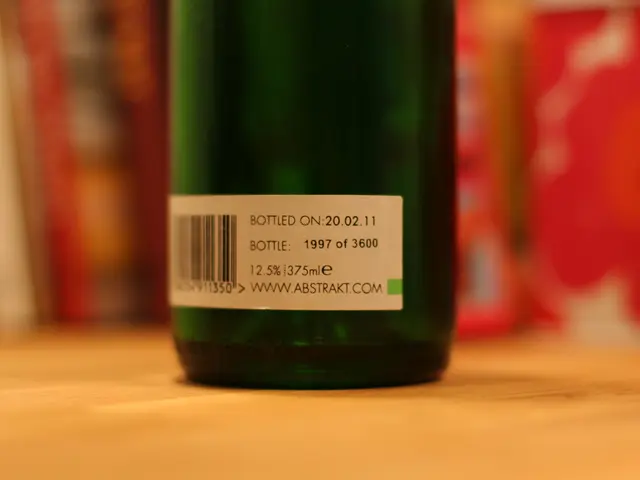
Other important considerations include storing PERT capsules at room temperature, avoiding crushing or chewing them, and not taking them on an empty stomach or with a hot drink. Antibiotic use can also cause symptoms to persist in some cases, and over-the-counter proton pump inhibitors (PPI) like lansoprazole (Prevacid), omeprazole (Prilosec), and esomeprazole (Nexium) may be recommended.
People with EPI may need vitamin or mineral supplements to prevent nutrient deficiencies, including vitamin A, vitamin D, vitamin E, and vitamin K. PERT is a treatment for EPI that requires a prescription, and untreated EPI can result in serious complications and even death. Eating small meals more regularly can help with PERT absorption.
Read also:
- Reversing Aging: Strategies for Restoring Vitality and Youthfulness
- Surgery and Chest Discomfort: Length and Remedies Exploration
- Challenging Lilly's dominance in the obesity drug market, five new oral medications are causing a stir. Orforglipron, Lilly's trademark drug, faces stiff competition.
- Bowel Cancer Stool Indications and Prognosis