Death, Decisions, and Digitization: Redefining Medical Ethics with Alena Buyx
"People generally avoid contemplating their own mortality"
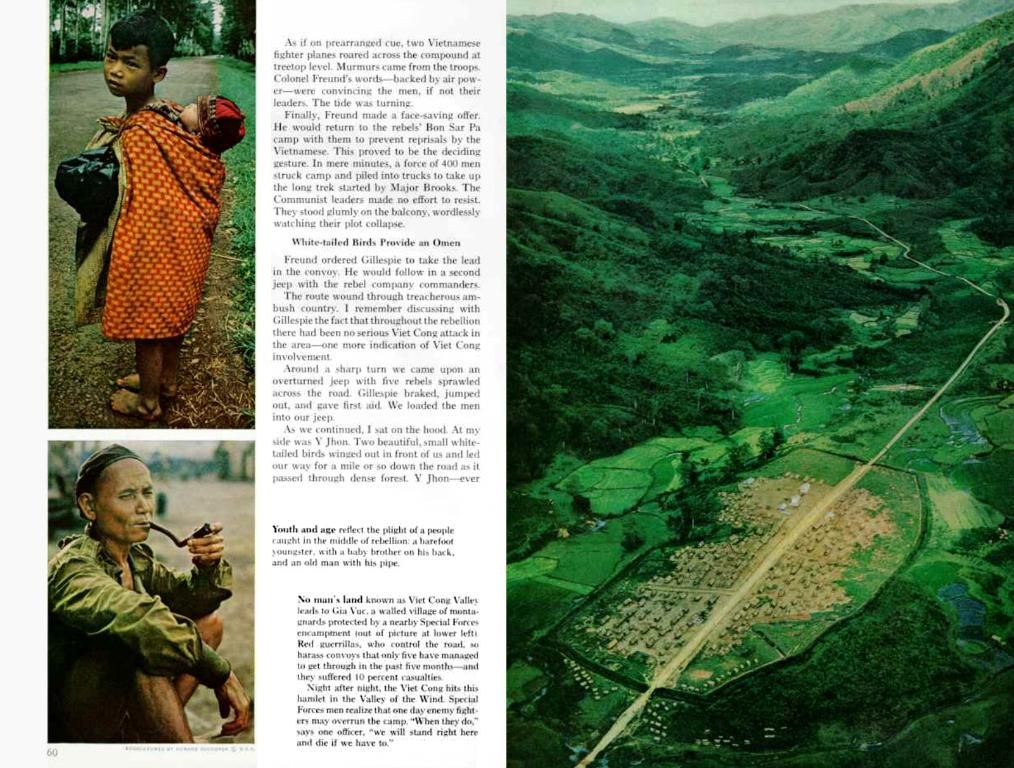
Alena Buyx, a renowned figure in the realm of medical ethics, discusses some of the most pressing ethical questions concerning life and death—queries that every individual must grapple with to some extent. Her latest book, "Life and Death," shines a light on these topics, prompting readers to think deeply about how they want to live and pass on.
ntv.de: What's the big question hanging over everyone's mind in the medical ethics realm at the moment?
According to Alena Buyx, it's essential to consider two primary questions: How do I want to live, and how do I want to die? The first question delves into the realm of personal lifestyle, medicine, health, and illness. The second question, naturally crucial in Buyx's field, concerns people's end-of-life care.
Surprisingly, many individuals shy away from making advance directives and appointing healthcare proxies, despite expressing a desire to determine their own fate.
Why is that?
Ignoring one's mortality is a common human tendency. Even organ donation, a generally popular concept, suffers from vague fears and inaction. Some worry about being simply switched off, while others hesitate due to misconceptions.
Is there truth to the fear of being turned off?
Studies have shown that clinical ethics consultation often results in patients living longer. Furthermore, Buyx observes that in the cases she's encountered, individuals are often treated beyond their desired duration.
What benefits can knowledge of these points bring when making decisions?
For the individual, proper preparation offers peace and clarity. Knowing a person's desires for their final stage of life makes decisions on their behalf more accessible, often a necessity. Different attitudes towards treatment can significantly impact the end-of-life experience, and open communication can help ease the process.
ntv.de: Five years of Corona in the "ntv Salon" Have we learned anything from the pandemic, Alena Buyx and Christian Drosten? What is changing?
While the pandemic can still be stressful and challenging, going through such experiences can provide a sense of preparedness and empowerment. This process doesn't have to be grim; it can be meaningful, especially when experienced collectively.
It's probably different for younger people facing accidents versus those nearing the end of their lives. How so?
The current life stage plays a significant role in decision-making. Older individuals or those with chronic illnesses may have different wishes when it comes to end-of-life care compared to younger, healthier individuals.
What advice would you offer for the elderly or those approaching the end of their lives?
Preventive care planning is crucial, especially for those dealing with illnesses or health issues. Seeking professional guidance is recommended for creating advance directives, patient declarations, and appointing healthcare proxies. Open conversations with family and friends about end-of-life wishes can also be beneficial.
It seems many people don't die peacefully at home. Are there ways to ensure a smooth end-of-life experience in a hospital setting?
Communication is key when expressing one's desires for end-of-life care. While coming with hard demands may not always be feasible, being open about preferences and working collaboratively with healthcare providers usually results in a positive outcome.
What role does religion play in these discussions, given that many people no longer rely on it as heavily as they once did?
Religious beliefs can still serve as a reservoir of influence in end-of-life decision-making, especially during existential crises. This is why religious arguments persist in the debates surrounding these topics.
To the offer at amazon.de
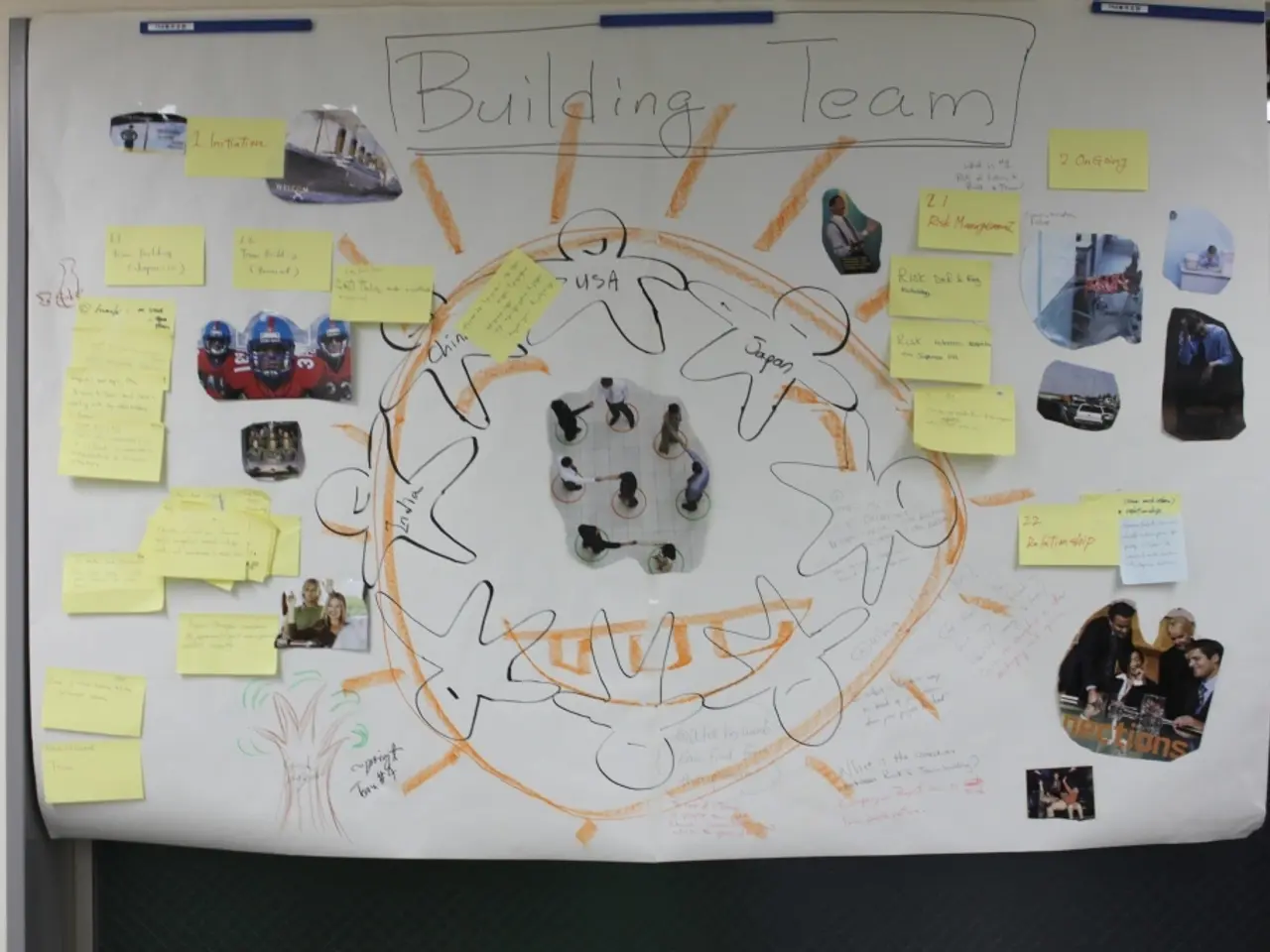
New biotechnological possibilities challenge ethical assessments within society, particularly concerning patient autonomy and control. Ethical debates on the use of AI and electronic health records (EHRs) revolve around informed consent and autonomy, algorithmic bias and fairness, patient-physician dynamics, patient acceptance, and oversight.
Ensuring transparency, fairness, and maintaining human aspects in this evolving landscape is crucial to addressing these ethical concerns.
- In the discussion on medical ethics, Alena Buyx highlights the importance of considering not only personal lifestyle decisions related to health, wellness, and illness, but also end-of-life care choices, which fall under the realm of health-and-wellness and mental-health.
- As healthcare evolves with technology, socio-ethical considerations surrounding patient autonomy, control, and informed consent in the context of AI and electronic health records (EHRs) are becoming increasingly important, raising questions about community policy and vocational training in the field of digital health.