struggles with Avoidant-Restrictive Food Intake Disorder (ARFID)
Eating Disorder Arfid: More Than Just Picky Eating
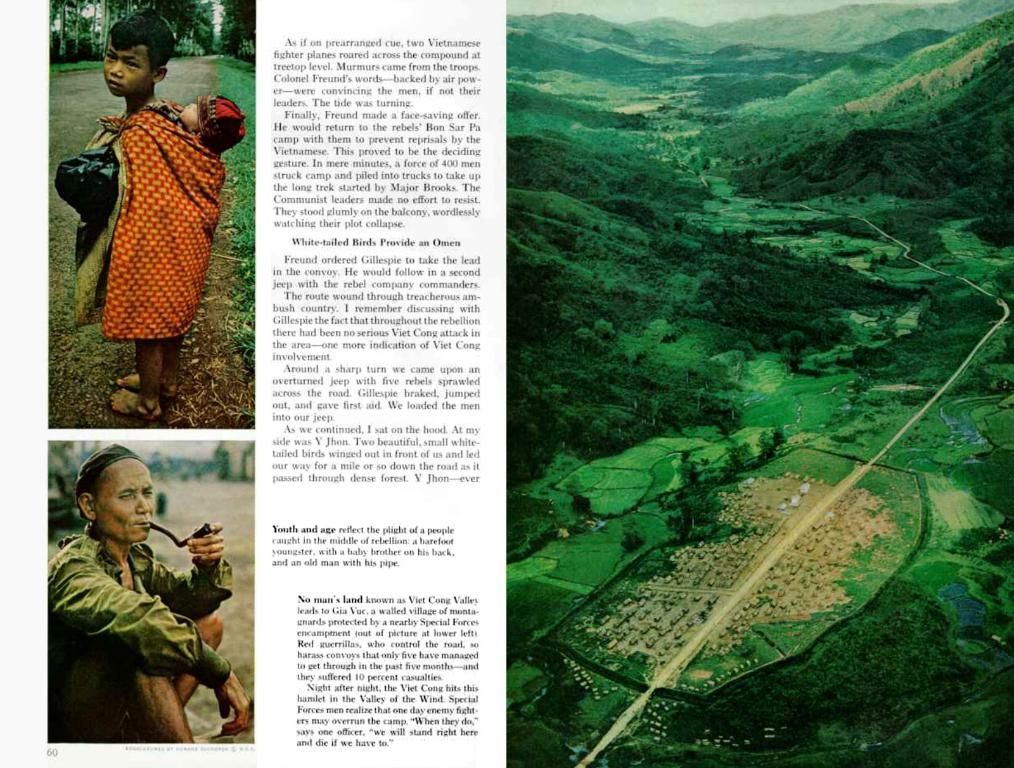
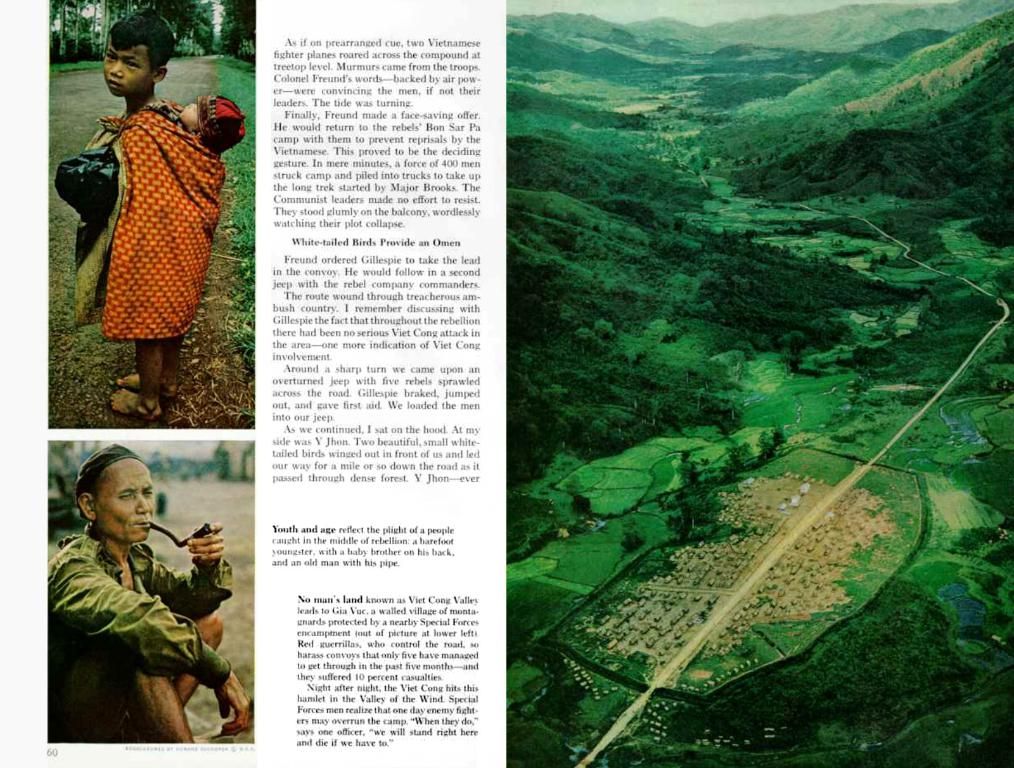
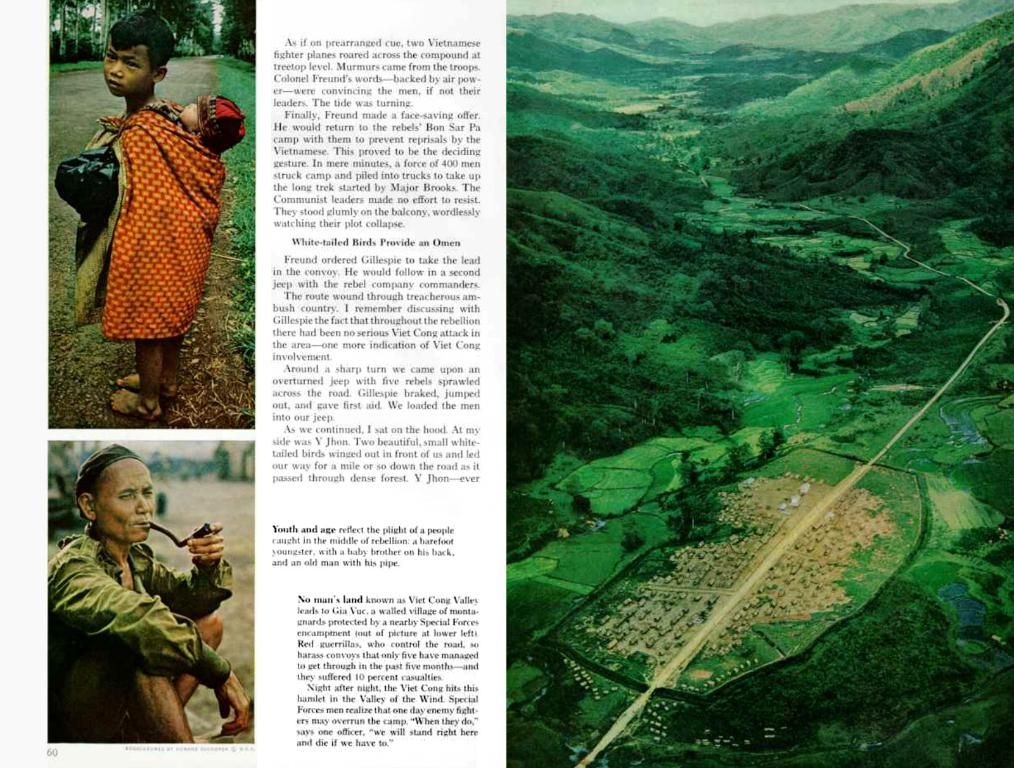
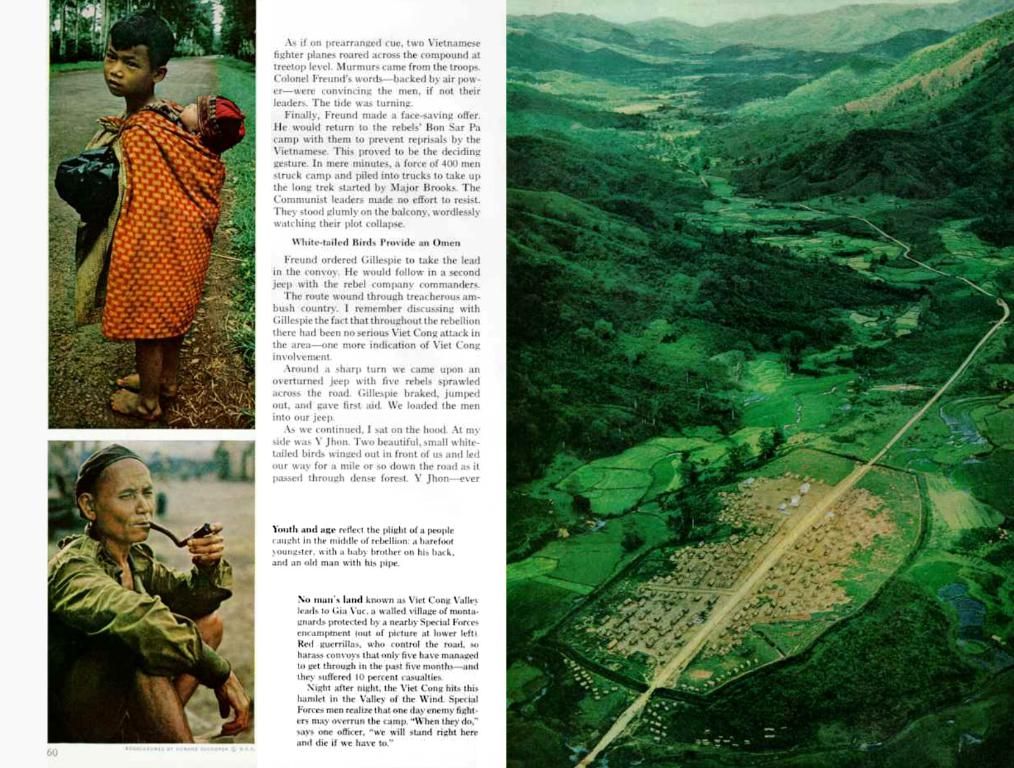
Mara, a woman in her mid-30s, has been living with the challenges of ARFID for most of her life. Similar to many others affected by this eating disorder, she struggles to consume solid fruits, vegetables, and cold cooked meats. As a result, social events like the company's Christmas dinner can cause considerable anxiety, naturally leading to sweaty palms and a feeling of being a toddler when it comes to food.
Before being formally diagnosed with ARFID, Mara believed her food-related issues were simply a sign of being stupid or childish. However, after seeing a post on Instagram about a child with similar eating behaviors, she discovered the term "Arfid." It was then she recognized that she, too, was dealing with this serious eating disorder.
ARFID, or Avoidant-restrictive food intake disorder, is not just about being picky with food. People with ARFID have a genuine inability to eat certain types of food due to specific sensory characteristics, such as smell, taste, texture, or appearance. In contrast, those who dislike certain foods can usually still consume them. Mara, for instance, can tolerate marzipan despite disliking the taste, but struggles with cooked ham due to its texture.
Mara now comprehends that she has a name for the disorder that has plagued her for about 30 years. This newfound knowledge provides relief. Although she maintains a healthy weight, she has consulted doctors and is considering seeking further assistance from psychotherapists or speech therapists, who may offer specialized support for aversions to specific solid foods.
Adults and children can both be affected by ARFID, according to Ricarda Schmidt, a psychosomatic medicine and psychotherapy expert at Leipzig University. Affected individuals may not feel hungry, have fearful eating habits, or exhibit little appetite. Schmidt notes that, for those with the disorder, eating is often viewed as a burden rather than an enjoyable activity.
The rejection of food can lead to malnutrition or weight loss in some extreme cases, as lack of proper nutrition impacts both physical and psychosocial well-being. In milder cases, individuals may avoid social gatherings, such as children's birthday parties or school trips, due to anxiety around the food choices presented.
While ARFID was first recognized in a diagnostic manual in the USA back in 2013, it has only recently gained recognition in Germany. The International Classification of Diseases (ICD-11) of the World Health Organization, which is not yet utilized in Germany, now includes ARFID. Doctors in Germany categorize appointments under "Other Eating Disorders." The exact number of individuals affected by ARFID is unknown, but a self-help association based in Münster exists to offer support.
Although specific therapeutic approaches for ARFID in Germany might be limited compared to other eating disorders, general trends and strategies used in the treatment of eating disorders can be applied. Treatment for ARFID often involves a multidisciplinary team, including psychologists, psychiatrists, nutritionists, and occupational therapists. These professionals collaborate to create personalized treatment plans addressing the physical, psychological, and social aspects of the disorder.
Family involvement is crucial in cases of ARFID, particularly for children and adolescents. Family-based therapy, including psychoeducational programs and family sessions, can help support parents in managing their child's food intake and other eating disorder symptoms. Psychotherapies such as cognitive-behavioral therapy (CBT) and exposure therapy are also commonly used to help individuals gradually become comfortable with a wider range of foods. In severe cases, nutritional support may be necessary to ensure proper nutrition.
ARFID can be stressful for the entire family, particularly when abnormalities in eating are noticed early on, such as during breastfeeding or when introducing solid foods. In such instances, parents are advised to consult a pediatrician to assess the physical consequences, including ruling out stomach and digestive problems or a food allergy. Proper support and guidance can help reduce the distress caused by ARFID.
While there are practical approaches to manage ARFID, it is essential to recognize that treatment does not aim to "cure" the disorder in a short period. Therapies may require around 60 sessions, and a longer-term commitment is often necessary for a balanced diet with adequate variety to be achieved.
Mara has made strides in expanding her food choices over time, now able to eat dried tomatoes and olives. Smaller steps, such as offering different pasta shapes or brands without adding sauce right away, can help children with ARFID to develop more varied eating habits. Positive reinforcement when previously rejected foods are consumed can also help to encourage increased food tolerance.
It is important for parents to stay patient and supportive in implementing these strategies. Little by little, children can be introduced to new foods, helping them overcome their fear and develop healthier eating habits.
Source: ntv.de, Simone Humml, dpa
Relevant Enrichment Data:
- Treatment for ARFID typically involves a multidisciplinary team, including psychologists, psychiatrists, nutritionists, and occupational therapists. These professionals work together to create personalized treatment plans addressing the physical, psychological, and social aspects of the disorder.
- Family involvement is crucial, especially for children and adolescents. Family-based therapy and psychoeducational programs can help support parents in managing their child's food intake and other eating disorder symptoms.
- Cognitive-behavioral therapy (CBT) and exposure therapy are often used to help individuals gradually become comfortable with a wider range of foods, reducing anxiety related to eating and increasing food acceptance.
- Nutritional support is essential, with such support including dietary counseling and addressing any nutritional deficiencies through supplements or tube feeding in severe cases.
Mara, being a part of the ARFID community, is considering seeking professional help from a multidisciplinary team comprising psychologists, psychiatrists, nutritionists, and occupational therapists, who may offer treatments tailored to her specific needs, considering the physical, psychological, and social aspects of her condition. In the realm of health-and-wellness, mental-health plays a significant role in Mara's case, as cognitive-behavioral therapy (CBT) and exposure therapy could potentially help her manage her food-related anxieties and gradually accept a broader variety of foods. Moreover, community support provided by self-help associations, such as the one based in Münster, could equally contribute to her well-being and recovery process.